0x00_读论文 8
0x11_算法平台 15
0x21_有监督学习 21
0x24_NLP 13
0x25_CV 11
0x26_torch 11
0x31_降维 10
0x33_图模型 9
0x43_时间序列 10
0x51_代数与分析 15
0x56_最优化 11
0x58_密码学 12
0x70_可视化 13
0x80_数据结构与算法 17
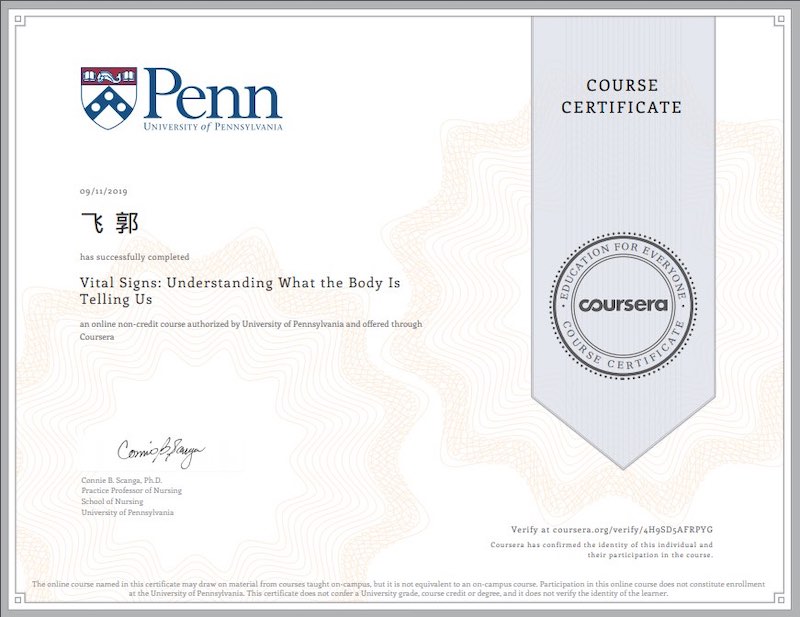
https://www.coursera.org/learn/vital-signs
Pulse Heart Rate
Video 1.1: Basic Heart Anatomy
The Heart’s Location within the Thoracic Cavity
- The heart is a hollow, muscular, cone-shaped organ
- General location
- Positioned in the mediastinum
- within the pericardial cavity
- between the pleural cavities
- enclosed by the pericardium
- function –anchors & protects the heart
- General location
- Esophagus and trachea are posterior to the heart
The Heart’s Internal Structure
- 4 chambers, or compartments
- Two superior chambers, or atria
- Two inferior chambers, or ventricles
- To prevent mixing of blood between chambers– interatrial septum and interventricular septum
- Ventricular walls are thicker than atrial walls because they are responsible for pumping blood into the systemic and pulmonary circulations
- Right atrium
- Receives deoxygenated blood from the body from three vessels
- Superior vena cava
- Inferior vena cava
- Coronary sinus
- From the right atrium, blood goes to the right ventricle
- Receives deoxygenated blood from the body from three vessels
- Right ventricle
- Pumps deoxygenated blood into the pulmonary trunk
- Left atrium
- receives oxygenated blood via the pulmonary veins m
- Left ventricle
- Pumps oxygenated blood into the aorta
- Left ventricular walls are thicker than right ventricular walls because they need to contract with more force in order to send blood throughout the systemic circulation
- The systemic circulation supplies the tissues and organs of the body with oxygenated blood
- the newly deoxygenated blood returns to the right atrium by the superior vena cava, inferior vena cava, and coronary sinus
Video 1.2a: Your Beating Heart
The Heart at a Microscopic Level
- 2 functional units (syncytia):
- the atrial syncytium
- the ventricular syncytium
- Atria contract, then ventricles contract, then the heart relaxes
- Two types of cells in the heart wall
- Contracting cells
- Cells that generate an electrical signal
- Form the cardiac conduction system:
- Occurs in each heartbeat
- Form the cardiac conduction system:
The Cardiac Conduction System
- Starts at the sinoatrial node(SA node)
- Location:
- Part of the cardiac conduction system that generates an electrical signal most rapidly
- Spreads signal over entire atrial syncytium causing atrial contraction
- Signal spreads to the atrioventricular node(AV node)
- Signal passes through the atrioventricular bundle(AV bundle)
- Signal arrives in the interventricular septum
- Passes through two bundle branches(right and left)
- At apex, the fibers branch extensively, forming Purkinje fibers
- Electrocardiograms(ECGs) assess the cardiac conduction system
- Determine if electrical activity of the heart is working properly
Video 1.2b: ECG Demo
- ECGs are devices we use to detect the electrical activity in the heart
- Electrodesare placed on the body
- 2 upper limb leads
- 2 lower limb leads
- 6 precordial leads
- Allows you to look at the heart from 12 different angles-\> can pinpoint location of abnormality, if present
- Electrodesare placed on the body
- The current arising from the SA node is a positive current, called depolarization
- The positive current passes through the atrial walls
- A negative current restores the electrical potential of the atrium back to normal after the passing of the positive current, this is called repolarization
- Normal Sinus Rhythm
- P wave: first wave
- QRS complex: second group of waves
- Consists of the Q, R, S waves
- T Wave: third wave
- Isoelectric lines–occur when there is no change occurring in the electrical state of the heart (i.e., no depolarization or repolarization is occurring)
- Between P wave and QRS complex
- Between QRS complex and T wave
Video 1.3a: Heart Valves, Part 1
- Heart valves ensure that blood flows in one direction through the heart
- Composed of dense, fibrous connective tissue
- covered in endocardium-
- Heart has 4 valves- organized as two pairs
- Atrioventricular valves(AV valves)
- tricuspid valve 右心房心室之间
- mitral valve 左心房心室之间
- Close when ventricles contract and the pressure in the ventricles exceeds pressure in the atria
- chordae tendinae:
- papillary muscles contract along with ventricles, creating tension in the chordae tendinae, preventing the free edges of the valves from swinging upward into the atria
- Open after ventricular relaxation, when atrial pressure exceeds ventricular pressure
- Semilunar valves (SL valves) :Blood passes from right ventricle to the pulmonary trunk and from the left ventricle into the aorta
- pulmonic valve
- aortic valve
- When closed, the cusps fall into the center of the pulmonary trunk and aorta to prevent backflow of blood from the vessel into the ventricle
- When the ventricles contract, pressure in them increases- when ventricular pressure exceeds pressure in the aorta and pulmonary trunk, the semilunar valves open
- When the ventricles relax, pressure drops- when the ventricular pressure falls below the pressure in the aorta and pulmonary trunk, the semilunar valves close
- Atrioventricular valves(AV valves)
Movement of valves during the cardiac cycle
- When the heart is relaxed
- the semilunar valves are closed and the AV valves are open
- blood is coming back to the right atrium through the superior vena cava, inferior vena cava and coronary sinus
- On the left side, blood is returning to the heart from the pulmonary veins from the lungs
- the semilunar valves are closed and the AV valves are open
- Atria contract
- Pressure in atria increases
- Atria relax, ventricles contract
- Pressure in ventricles exceeds pressure in atria
- Pressure continues to climb as ventricles continue to contract -\> ventricular pressure exceeds pressure in aorta and pulmonary trunk
- Ventricles stop contracting, start to relax
- Cycle repeats
- When valves close, they cause vibrations to occur in the blood that's passing through the heart
- Vibrations are carried to the body's surface and can be heard with a stethoscope
- sound one:
- sound two:
Video 1.3c, Assessing Heart Rate Demo
- Auscultation:
- The heart is positioned deep to the sternum, slightly to the left of the midline in the chest cavity
- the apex:
- Location:
- Orientation:
- point of maximal impulse- the most accurate place to check heart rate
- the apex:
- Feeling the heart rate, or palpating, assesses the number of beats per minute
- Auscultation allows assessment of heart rate as well as heart sounds
- Heart sounds include sound oneand sound two, usually called S1an S2
- S1
- S2
- Heart sounds include sound oneand sound two, usually called S1an S2
- Physicians often auscultate in multiple locations to assess heart sounds related to the specific valves
- aortic valve:
- pulmonic valve:
- tricuspid valve:
- mitral valve:
- If a valve does not close all of the way, it will make a swishing sound
- If a valve does not open all of the way, it will make a clicking sound
Video 1.4a, The Cardiac Cycle, Part 1
Electrical Changes During the Cardiac Cycle
- Conduction system:
- Starts at the SA node
- Excitation of the atria creates the P-wave on an ECG
- Signal sent to the AV node
- Delayed for 1/10 th of a second—
- Passed to AV bundle
- The only electrical connection between the atrial syncytium and ventricular syncytium
- Excitation of the ventricles creates the QRS complex on an ECG
- Heart relaxes, ventricles repolarize
- Creates the T wave on the ECG
- Starts at the SA node
- These electrical signals create changes in the contracting cells, triggering muscle contraction
Video 1.4b: The Cardiac Cycle, Part 2
Pressure Changes During the Cardiac Cycle
- Pressure changes in the heart cause the valves to open and close, to prevent backflow of blood
- The P wave on an ECG is followed closely by an increase in atrial pressure
- atrial contraction, atrial systole
- After atrial systole, the atria contract and pressure remains low
- The QRS complex on an ECG is followed almost immediately by an increase in ventricular pressure
- The period of ventricular contraction is called ventricular systole
- When ventricular pressure exceeds aortic pressure, the semilunar valves open
- Once this pressure peaks, the ventricles stop contracting
- Pressure in ventricles falls below the pressure in the aorta and pulmonary trunk
- The ventricles continue to relax and ventricular pressure continues to fall
- When this pressure falls below atrial pressure, the AV valves open
- The period when the ventricles are relaxed is called ventricular diastole–during this phase, ventricles fill with blood
- Once this pressure peaks, the ventricles stop contracting
- The P wave on an ECG is followed closely by an increase in atrial pressure
Ventricular Volume During the Cardiac Cycle
- Ventricular volume is fairly high during relaxation, or diastole
- During atrial systole- a little more blood is pushed into the ventricles, so the volume increases slightly
- Ventricles contract, pressure increases and volume decreases
- Blood is being ejected to the aorta and pulmonary trunk
- AV valves open and ventricular volume begins to increase again
Heart Sounds During the Cardiac Cycle
- Heart sound one indicates the start of ventricular systole
- Heart sound two indicates start of ventricular diastole
Video 1.4c: Assessing Pulse Demo
- Heart rate:
- Pulse:
- We assess pulse in elastic arteries, which can distend and retract
- Pulse and heart rate are typically the same in a person with healthy cardiovascular function, but could be different if someone has poor peripheral circulation or arterial disease
Locations to assess pulse:
- carotid artery
- brachial artery(at the antecubitalfossa)
- radial artery
- femoral artery
- dorsalis pedis
- posterior tibial
Video 1.5: Cardiac Output
- Need to keep blood circulating through the body to supply the cells with oxygen and nutrients and to carry away metabolic waste products
- Cardiac Output (CO)= the volume of blood ejected per minute
- Influenced by heart rate (HR) and stroke volume (SV)
- CO = HR x SV
- Stroke volume: the volume of blood ejected during a single heartbeat
- End diastolic volume(EDV):
- End systolic volume(ESV):
- Stroke volume = EDV - ESV
- Cardiac output can be increased or decreased to meet the needs of the body
- The autonomic nervous system plays a role in regulating cardiac output
- Two branches : parasympatheticand sympathetic
- sympathetic division:
- in the heart, the sympathetic nervous system innervates SA node, AV node and the contractile cells of the myocardium
- when activated, causes the SA node to depolarize more quickly and can shorten the delay at the AV node
- tachycardia= HR \>100 bpm
- sympathetic activation also causes contractile cells of myocardium to contract more forcefully -\> leads to increased stroke volume
- parasympathetic division:
- in the heart, the parasympathetic nervous system innervates the SA node & the AV node
- parasympathetic nervous system slows the SA node's rate of self-excitation
- parasympathetic signals are carried to the SA node by the vagus nerve
- bradycardia= HR \< 60 bpm
- sympathetic division:
- Two branches : parasympatheticand sympathetic
Blood Pressure
Video 2.1: Introduction to the Blood Vessels
Anatomy of the blood vessels
- Five types of blood vessels:
- arteries
- arterioles
- capillaries – site of gas exchange
- venules
- veins
- Two circulations
- Systemic circulation:
- arteries carry blood to capillaries
- in the capillary beds, oxygen (O2 )leaves blood and moves to tissues and carbon dioxide (CO2) moves from the tissues to the blood
- deoxygenated blood is then brought back to the right side of the heart through systemic veins
- aorta carries blood into the systemic circulation
- aorta branches into smaller arteries
- branching continues until vessels are small enough that they are called arterioles
- small arterioles carry blood to capillaries
- capillaries converge to form venules
- venules converge and form veins
- Systemic circulation:
- Pulmonary circulation:
- pulmonary trunk carries deoxygenated blood into the pulmonary circulation
- it branches into R. & L. pulmonary arteries, which carry blood to the R. & L. lungs, respectively
- gas exchange occurs in pulmonary capillaries
- pulmonary veins carry oxygenatedblood back to the left side of the heart
- pulmonary trunk carries deoxygenated blood into the pulmonary circulation
Video 2.2: Blood Vessel Structure
All blood vessels except the capillaries have walls consisting of 3 layers
- tunica intima
- innermost layer is called endothelium – it is continuous with endocardiumf the heart
- thin, smooth tissue – low friction for blood flow
- directly surrounds the lumen :
- endothelium is the only tissue layer in capillaries
- tunica media
- contains many elastic and smooth muscle fibers
- elastic fibers - able to distend and retract
- smooth muscle is arranged in concentric layers around the wall of the vessel
- when the smooth muscle contracts, it causes the vessel diameter to decrease in size –this is called vasoconstriction
- conversely, when the smooth muscle relaxes, the vessel diameter increases –this is called vasodilation
- innervated by the sympathetic nervous system
- even at rest, the sympathetic nervous system is sending signals to the vascular smooth muscle, causing a baseline level of vasoconstriction
- higher level of sympathetic outflow, cause greater stimulation of the smooth muscle which can cause greater amount of vasoconstriction
- contains many elastic and smooth muscle fibers
- tunica externa
- made of a layer of connective tissue
- anchors the blood vessel in place and helps protect the outside of the vessel
Specific Type of Blood Vessels- Structure and Function
- 3 general types of arteries:
- elastic arteries
- closest to heart
- tunica media contains relatively more elastic fibers
- these large arteries have to be able to distend during ventricular systole to compensate for the surge of blood
- then, the vessels retract during diastole, maintaining pressure which allows for a continuous flow of blood
- atherosclerosis
- muscular arteries
- tunica media contains more smooth muscle
- because there is more smooth muscle in the vessel walls, these vessels have a greater ability to vasoconstrict or vasodilate,, which allows them to channel blood to different organs or regions of the body
- arterioles
- large amount of smooth muscle in tunica media
- very responsive to signals from the sympathetic nervous system in terms of vasoconstricting or vasodilating
- these vessels have a big impact on vascular resistance
- large amount of smooth muscle in tunica media
- elastic arteries
- veins
- venous walls are always thinner than an arterial wall that is the same distance away from the heart
- thin, collapsible walls which distend and collapse easily
- veins have relatively large lumen diameters
- due to the structure of veins, venous pressure is low
Video 2.3: Blood Circulation
Blood Circulation
- heart beats intermittently yet blood flows continuously(因为血管会突然舒张,以降低心脏负担;缓慢搜索,以稳定流动)
- blood flow =volume of blood that moves through a level of the vascular system per minute
- blood flow is equal to cardiac output (CO)
- blood flow is fairly constant under resting conditions
- blood pressure = force exerted per unit of surface area against the inner walls of a blood vessel
- unit of measurement is millimeters of mercury (mmHg)
- blood flows from region of high pressure to region of low pressure
- resistance = anything that opposes, or impedes, blood flow
- most resistance is in the systemic circulation, away from heart –called peripheral resistance
- influenced by several factors:
- vessel diameter
- #1 factor responsible for changes in vascular resistance
- arterioles are most responsible for changes in peripheral resistance
- blood viscosity- thickness or thinness of the blood
- is fairly constant in healthy people
- anemia
- polycythemia
- is fairly constant in healthy people
- vessel length
- pulmonary vs. systemic circulation-
- vessel diameter
Video 2.4a: Maintaining Blood Flow
- pressure gradient –difference in pressure from one part of the vascular system to another
- blood flows down its pressure gradient
- pressure across the systemic circulation
- systolic pressure (SBP)
- generated by ventricular contraction
- = the highest pressure achieved in the large arteries
- diastolic pressure (DBP)
- achieved during ventricular relaxation
- = the lowest pressure in the large arteries, achieved at the end of ventricular diastole
- during diastole, elastic arteries retract to maintain pressure –diastolic pressure is lower than systolic pressure
- mean arterial pressure (MAP)
- highest MAP occurs in large arteries
- lower in smaller arteries due to increased resistance
- decreases across the capillary beds
- lowest in the large veins close to the heart
- systolic pressure (SBP)
- MAP continues to drop in the veins- several features help to maintain blood flow through the veins even though pressure is low
- venous valves –prevent backward flow of blood
- skeletal muscles
- muscles bulge when contracted – pushes on veins to send blood to heart
- then, during muscular relaxation, venous valves prevent backflow
- pressure changes in the thoracic cavity during breathing –lower thoracic cavity pressure during inhalation helps return blood to the heart
Video 2.4b: Assessing Blood Pressure Demonstration
To take a blood pressure:
- gather necessary equipment:
- inflatable cuff attached to a sphygmomanometer
- make sure the cuff is the correct size –if cuff size is wrong, the BP readings will not be accurate
- stethoscope
- inflatable cuff attached to a sphygmomanometer
- apply the cuff-
- line up artery marker with brachial artery
- cuff bottom should be in crook of the elbow (i.e., the antecubital fossa)
- taking the pressure
- ideally, take the reading in the left arm and support the arm at the same level of the heart to get the most accurate reading
- inflate the pump – this will cause cuff to inflate, occluding arteries under the cuff
- arteries collapse, preventing blood flow
- release gauge to deflate cuff
- listen to brachial artery – will be quiet until blood flow is no longer occluded
- Korotkoff sounds
- note first sound and last sound
- systolic pressure –corresponds to the first Korotkoff sound
- diastolic pressure –sound of turbulent flow stops because blood is flowing smoothly through the artery again
- blood pressure reading of 110 over 62 (110/62) –SBP is top number, DBP is bottom number
Video 2.5: Blood Pressure Regulation
Normal and abnormal blood pressure
- In healthy adults, systolic blood pressure should be no higher than 120 mmHg and diastolic should be less than 80 mmHg
- low blood pressure (hypotension)
- typically not a problem unless it interferes with the ability to carry blood to the tissues
- hypertension—i.e., high blood pressure
- can cause damage to blood vessel endothelium
- ver time, leads to narrowing of lumen and blood flow restriction
- damage to heart
- increased workload
- structural changes
- we can have hypertension and not experience symptoms –because untreated hypertension can damage the cardiovascular system, it is important to have BP assessed regularly and treat hypertension
- can cause damage to blood vessel endothelium
Factors affecting mean arterial pressure
- cardiac output
- resistance
- arterioles create the most vascular resistance
- cardiovascular regulatory centers—in brainstem
- receive input from baroreceptors –these are sensors in blood vessel walls that detect the level of stretch in the blood vessel walls
- regulate pressure by changing vessel diameter and cardiac output
- blood volume
- normally is fairly constant
- long term mechanisms involving hormonal regulation and kidney function can change blood volume which then lead to changes in blood pressure
Metabolism
Video 3.1: Introduction to Metabolism
- metabolism –the combination of chemical reactions occurring in the body
- two general types of chemical reactions comprise metabolism:
- catabolism (decomposition reaction)
- anabolism - (building reactions)
- sum of all reactions metabolic rate
- two general types of chemical reactions comprise metabolism:
- macronutrients are used to fuel the body-
- fats-
- triglycerides are the main dietary fat
- made of mono glycerol and fatty acids
- carbohydrates
- sugars and starches
- after digestion, we absorb simple sugars
- primarily used to supply energy (ATP) to the body's cells
- proteins
- made of amino acids
- used to build cellular proteins (e.g., muscle proteins) and can also be used catabolically to provide energy for the body
- fats-
- after digestion, nutrients enter the blood and become part of the nutrient pool
- macronutrients are used to create cellular energy in the form of adenosine triphosphate (ATP) through cellular respiration
- ATP is used to directly supply energy for chemical reactions that take place in the cells
Video 3.2a: Cellular Respiration, part 1
- cellular respiration -
- begins with glycolysis-
- glucose is broken down into pyruvic acid, then further converted (into acetyl-coA) and channeled to the Krebs Cycle
- this set of reactions occurs in the cytoplasm of the cells
- Krebs cycle
- produces molecules that can be taken into the electron transport chain
- ccurs in the mitochondria of the cells –produces CO2
- oxidative phosphorylation
- ccurs in the electron transport chain (also in the mitochondria)
- yields a large amount of ATP –this is where O2 is used and H2O is generated
- begins with glycolysis-
- amino acids
- usually used anabolically to build new protein
- can also be channeled into catabolic pathways and use for ATP production
- triglycerides, our main dietary lipid,are broken into
- glycerol – enters glycolysis
- fatty acids – converted to acetyl-CoA and channeled into the Krebs cycle
Video 3.2b: Cellular Respiration, part 2
-
the glycolytic pathway can end two ways:
- pyruvic acid
- end product of glycolysis when sufficient O2 is available
- gets channeled into the Kreb's cycle
- lactic acid
- forms when insufficient O2 is available
- not a waste product
- cardiac muscle cells can use lactic acid -\> convert back to pyruvic acid to use in the Kreb's cycle
- liver can use lactic acid to build new glucose molecules
- cellular respiration summarized chemically by the formula
- C6H12O6(glucose) + 6 O2(oxygen) —> 6 H2O(water) + 6 CO2(carbon dioxide) + up to 30 ATP
- if insufficient oxygen, glycolysis yields 2 lactic acid + 2 ATP
- ATP- adenosine molecule with phosphate groups attached
- 2 terminal phosphate groups are attached to the molecule with high-energy phosphate bonds
- cellular respiration is not totally efficient at capturing the energy stored in a fuel –as a result heat is also released
Video 3.3: Assessing Metabolic Rate Demonstration
- assessing metabolic rate
- measure oxygen consumption and carbon dioxide production
- oxygen consumption (VO2) is proportional to ATP production
- VO2
- respiratory exchange ratio (RER)
- RER –is calculated as follows VCO2/VO2
- where VCO2 = the rate of CO2 production and VO2 = the rate of O2 consumption
- can be used to determine what type of substrate is being consumed
- ranges from 0.7 to 1
- an RER of 0.7 indicates that fats are the main fuel source
- higher ratio tells us a greater proportion of carbohydrates are being consumed
- an RER of 1.0 or higher indicates that carbohydrates are the predominant fuel source
- RER –is calculated as follows VCO2/VO2
- METs = metabolic rate (actually stands for "metabolic equivalent of task")
- METs increase as energy consumption increases
- 1 MET represents a resting metabolic rate
- 6 METs indicates that one's metabolic rate is 6 times higher than the metabolic rate at rest
- during vigorous exercise, MET level can rise to 12-20
- when the MET level goes up, heat production will also increase
- METs increase as energy consumption increases
Video 3.4: Metabolic Lab Discussion
- resting metabolic rate
- metabolic rate increases with activity
- VO2 and VCO2 increase –as a result of the increase in cellular respiration
- respiratory rate increases \> more gas exchange in lungs
Body Temperature
Video 4.1: Introduction to Thermoregulation
- metabolic rate: measure of all of the chemical reactions going on in the body at a given time
- certain organs have continuous rate of metabolism that contributes significantly to establishing our resting metabolic rate –e.g., the heart, brain, liver, kidneys
- body core –the internal region of body where we normally maintain a fairly constant temperature
- heat is released with an increase in metabolic rate because cells are not 100% efficient –increased metabolism, as occurs during exercise, creates more heat
- core body temperature-
- normal range : 35.8°C-38.2°C
- normal core temperatures vary between individuals and throughout the day
- lowest during-
- highest during-
- important to maintain a normal temperature for optimal enzyme activity-
- body shell
- more temperature fluctuation occurs in the body shell
- based on atmospheric temperature and body's metabolic rate
- blood – mechanism of heat transfer in body
- picks up heat in body core \> carries heat to less metabolically active parts of body
- more temperature fluctuation occurs in the body shell
- types of heat transfer:
- conduction
- radiation
- convection
- body heat will transfer to the cold fluid, which will then rise away from the body surface and be replaced by cooler fluid
- the cooler fluid will warm (due to heat transfer from the body) –and then it will rise away from the body surface
- the greater the temperature gradient between the body and the cool fluid that replaces the warm fluid, the greater will be the heat loss
- wind chill
- evaporation
- heat is required to vaporize water (called the "heat of vaporization")
- it is not sweating per se that makes us feel cooler –it is the evaporation of sweat that cools us
- when sweat evaporates, it is body heat that vaporizes the water in sweat
- heat index
- heat is required to vaporize water (called the "heat of vaporization")
- heat loss from the body can be sensible or insensible:
- sensible heat loss-
- example: sweating
- insensible heat loss-
- example: evaporation that occurs as air moves past the airway surfaces during inhalation
- sensible heat loss-
Video 4.2: Maintaining Body Temperature
Reflex arc:
- all reflex arcs begin with a sensory receptor –the temperature sensors of the body are called thermoreceptors
- peripheral thermoreceptors
- sensitive to hot and cold
- peripheral thermoreceptors provide the information which helps us cope with environmental temperature changes
- body has high water content which creates thermal inertia –peripheral thermoreceptors make the brain aware of changes in environmental temperature so that adjustments can be made to maintain core temperature
- central thermoreceptors
- peripheral thermoreceptors
- neurons carry the sensory input to the hypothalamus , which is the control center for body temperature regulation
- temperature control center is located in the preoptic nucleus of the hypothalamus
- motor effects allow us to maintain our temperature
- temperature homeostasis –state of dynamic equilibrium in which we maintain our body core temperature within the normal range (35.8°C-38.2°C)
- decreased body temperature –when body temperature falls below the hypothalamic set point it causes:
- vasoconstriction of subcutaneous blood vessels
- shivering-
- the slight shaking or shuddering that we call "shivering" is due to rapid involuntary muscle contractions
- remember: about 60% of the energy stored in the molecular bonds of fuel molecules is released as heat
- thus, as skeletal muscles generate ATP to fuel shivering, they also generate a lot of heat
- hormonal secretion
- in prolonged cold, hormones can stimulate metabolism & help to maintain a normal body temperature
- increased body temperature – body/blood is warmer than the hypothalamic set point
- vasodilation of subcutaneous blood vessels
- increases heat loss via radiation (and possibly convection)
- sweating
- vasodilation of subcutaneous blood vessels
- negative feedback is built into the temperature regulating system
Video 4.3: Hypothermia & Hyperthermia
- hypothermia – condition in which the body core temperature falls below the normal range
- normal physiological mechanisms to warm body (constriction of subcutaneous blood vessels, shivering) are not enough to raise body temperature back to the normal range
- manifestations-
- decreased heart rate
- decreased respiration rate
- decreased blood pressure
- brain functions will also begin to fail if the hypothermia become severe enough and/or prolonged
- interventions-
- hyperthermia:
- varies in severity
- heat exhaustion
- blood cannot circulate effectively due to blood volume loss from excessive sweating
- conflicting signals
- can occur after prolonged exercise in heat
- manifestations
- interventions:
- heat stroke –condition is more severe than heat exhaustion
- positive feedback cycle created that generates heat loss mechanisms that worsen the condition
- manifestations:
- hot, dry skin
- rgans shut down (i.e., organ failure)
- predisposing factors can put some people at higher risk:
- lder adults
- young children and neonates
- people with cardiovascular disease-
- pregnant women-
- people who have impaired fluid regulation capability (as in chronic kidney failure)-
- interventions:
- heat exhaustion
Video 4.4: Fever
- Fever:
- pyrogens – molecules released by the cells of the immune system that have the ability to raise the hypothalamic set point
- released by cells of the immune system (mainly) and can circulate in the blood
- when they arrive in the brain, they affect hypothalamic function
- when hypothalamus set point is increased, the higher body temperature of a fever is interpreted by the hypothalamus as "normal"
- may feel cool despite high temperature
- a fever "breaks" when the pyrogens are removed from body and hypothalamus returns to normal set point
- fever is not always a bad thing
Video 4.5: Assessing Body Temperature Demo
- Types of thermometers-
- oral
- place probe of thermometer in sublingual pocket-
- close to sublingual artery – a deep artery, which gives a more accurate measure of core body temperature
- place probe of thermometer in sublingual pocket-
- temporal
- run probe over patient's forehead –assesses temperature in temporal artery , which also carries blood a short distance from the core and gives a relatively accurate measure of core temperature
- tympanic
- placed in external auditory canal against tympanic membrane (or ear drum)
- close to hypothalamus –thus, gives a fairly accurate measure of core temperature
- placed in external auditory canal against tympanic membrane (or ear drum)
- axillary
- measured in axilla (or armpit)
- it is difficult to get an accurate reading at this site, for various reasons
- measured in axilla (or armpit)
- rectal
- sensor probe is placed in rectum
- requires practice and training for accurate readings
- oral
- important to take a temperature when patient is healthy –then, are able to compare future readings to this baseline temperature
Respiration Rate
Video 5.1: Basic Anatomy of the Respiratory System
- Respiratory system:
- nares (nostrils)
- nasal cavity
- pharynx
- nasopharynx
- ropharynx
- laryngopharynx
- larynx
- epiglottis
- during swallowing, the epiglottis covers the opening through the larynx to direct what is swallowed to the esophagus
- epiglottis
- trachea
- divides to form the right and left primary bronchi
- primary bronchi branch for form secondary bronchi
- 2 left secondary bronchi
- 3 right secondary bronchi
Video 5.2: Anatomy of Ventilation
- ventilation
- inhalation-
- chest wall moves out and up, stretching the elastic tissue
- inhalation is an active process-
- quiet inspiration –involves contraction of:
- diaphragm-
- external intercostal muscles
- forced inspiration
- requires contraction of additional skeletal muscles
- these accessory muscles are:
- sternocleidomastoid
- scalenes
- pectoralis minor
- quiet inspiration –involves contraction of:
- exhalation-
- chest wall moves down and in
- quiet exhalation is a passive process- elastic tissue retracts to normal position
- exhalation becomes an active process, too, if one is breathing vigorously
- forceful exhalation –skeletal muscles involved:
- muscles of the abdominal wall
- internal intercostals
- inhalation-
- pleura
- pleurae are one example of a serous membrane- thin membrane layer that covers the outer surface of organs in the body cavity, then reflects outward to line the cavity
- visceral pleura
- parietal pleura
- pleural cavity –a thin potential space which is filled with pleural fluid that is secreted by the pleural membranes –
- creates adhesive force-
- pleurae are one example of a serous membrane- thin membrane layer that covers the outer surface of organs in the body cavity, then reflects outward to line the cavity
Video 5.3: The Mechanics of Breathing
- Inhalation-
- lung volume increases - decrease in intrapulmonary pressure
- when intrapulmonary pressure is less than atmospheric pressure, air flows into lungs
- Exhalation-
- lung volume decreases - increase in intrapulmonary pressure
- when intrapulmonary pressure is greater than atmospheric pressure, air flows out of the lungs
- spirometry tracing:
- tidal volume –average adult tidal volume = 500 mL
- inspiratory reserve volume
- expiratory reserve volume
- vital capacity
- residual volume –volume of air left in the lungs at the end of a forceful exhalation
- keeps alveoli open –makes it easier to take the next breath
- a greater resistance in the respiratory system makes it more difficult to move air in and out of the airways
- bronchoconstriction:
- parasympathetic nervous system-
- bronchodilation:
- sympathetic nervous system-
- bronchoconstriction:
Video 5.4: Gas Exchange
Gas exchange
- alveoli –the air pockets of the lungs, site of gas exchange
- each alveolus has a very thin wall surrounded by a dense network of capillaries
- gas exchange takes place across the respiratory membrane
- layers of the respiratory membrane
- O2 and CO2 move across the respiratory membrane via the process of diffusion
- concentrations of gases in a mixture is measured as partial pressures -
- each gas (O2 and CO2) diffuses down its own partial pressure gradient
- as deoxygenated blood flows into the pulmonary capillaries
- partial pressure of O2 is relatively lower
- partial pressure of CO2 is relatively higher
- gas exchange occurs in the pulmonary capillaries, and oxygenated blood then flows into the pulmonary veins
- partial pressure of O2 is high
- partial pressure of CO2 is lower
- as oxygenated blood flows into the systemic capillaries
- partial pressure of O2 is high
- partial pressure of CO2 is relatively low
- gas exchange occurs in the systemic capillaries, and deoxygenated blood flows into the systemic veins
- partial pressure of O2 is lower
- partial pressure of CO2 is relatively high
Video 5.5: Regulating Respiration Rate
Control of respiration rate:
- chemoreceptors –the specialized chemoreceptors that monitor changes in O2, CO2, and pH of body fluids
- they are categorized as peripheral or central chemoreceptors
- peripheral chemoreceptors
- located in the aortic and carotid bodies
- monitor the chemistry of systemic arterial blood
- central chemoreceptors
- in the brainstem near the control centers for respiration rate
- monitor changes in the cerebrospinal fluid
- cerebrospinal fluid is separated from the blood by the blood brain barrier
- normally, central chemoreceptors play the main role in regulating respiration rate
- peripheral chemoreceptors
- they are categorized as peripheral or central chemoreceptors
- chemical factors influencing respiration
- carbon dioxide
- increased pCO2 in systemic arterial blood is the most powerful stimulus for regulation of respiration rate
- it is the central chemoreceptors that are most sensitive to increased pCO2 in arterial blood
- however, the increased pCO2 affects the central chemoreceptors indirectly –by causing the pH of the cerebrospinal fluid to decrease
- oxygen
- pO2 may fall low enough to stimulate respiration in certain clinical situations (i.e. pneumonia, congestive heart failure)
- it is peripheral chemoreceptors that are most responsive to increased pO2 in arterial blood
- pH
- acids (free H+) are generated in the body via metabolism
- examples of these types of acids are lactic acid & ketoacids
- peripheral receptors are most responsive to the decreased pH associated with accumulation of metabolic acids
- carbon dioxide
- regulating respiration
- when chemoreceptors are activated, they increase activation of respiratory centers in the medulla of the brainstem
- this results in increased neural impulses to respiratory muscles
-
under normal circumstances, the indirect activation of central chemoreceptors by the increased pCO2 of systemic arterial is the primary stimulus regulating respiration
- chronic obstructive pulmonary disease (COPD) –condition in which there is impaired recoil ability of lung tissue
- also, in patients with COPD, there is a destruction of alveolar walls - enlarged air pockets
- these enlarged air pockets cause increased dead space in lungs –i.e., these spaces are not involved in gas exchange
- slower, deeper breaths (versus shallow, rapid breaths) is more efficient at getting more fresh gas into the alveoli
- if recoil properties are impaired, however, it may not be possible to breath efficiently
Video 5.6: Assessing Respiration Rate Demonstration
- subject should be comfortable & relaxed to get a baseline respiration rate
- there is a large range of respirations rate –on average, normal range is 15-20 breaths per minute in adults
- physical activity and emotional stress can cause an increased respiration rate
- respiration rate is slowed, or depressed, in certain periods of sleep and in hypothermia
-
certain medications may also alter breathing rate
- clinically speaking, the quality of the subject/patient's breathing is also important
- is the person having labored breathing, are they short of breath, do they wheeze or cough while breathing
- when someone has to engage accessory muscles to accomplish quiet breathing, this person is working harder than normal to breath
Video 5.7: Regulating Respiration Rate Review
- two types of chemoreceptors-
- central chemoreceptors:
- peripheral chemoreceptors:
- primary controls of respiration:
- pCO **2** -
- the most powerful stimulus for respiration
- affects central chemoreceptors by crossing the blood brain barrier –causes an increased formation of carbonic acid in the CSF increased formation of free H+ (decreased pH) -** pH-** -** O **2 –
- low pO2 stimulates peripheral chemoreceptors to increase respiration rate
- pCO **2** -
Video 5.7: Assessing Breath Sounds Demo
- assess to see if breath sounds are normal or abnormal (i.e., adventitious )
- there are several different types of adventitious breath sounds
- have patient take a deep breath when auscultating-
- review of lung anatomy:
- right lung has three lobes –upper, middle & lower lobes
- left lung has two lobes –upper & lower lobes
- have subject take deeps breaths while you move stethoscope around, in a ladder pattern, so you can listen at multiple sites
- review of lung anatomy:
- types of abnormal sounds
- crackles(rales)–could hear when patient has pneumonia or pulmonary edema (fluid accumulation in the lungs)
- wheezing –common to hear this sound when someone has asthma
Pain
Video 6.1: The Anatomy&Physiology of Pain, Part 1
- Introduction to pain
- the symptom most likely to inspire people to seek medical care
- defined as a sensory & emotional experience that is unpleasant and has the role of alerting us to potential damage to the body or body tissues
- there are different qualities and experiences of pain
- Sensory experience of pain
- the nervous system has 2 arms
- sensory –which consists of receptors and nerve fibers (carried in nerves) that conduct impulses/information toward the spinal cord & brain
- motor –consists of nerve fibers (carried in nerves) that conduct impulses to effectors (effectors are either muscles or glands)
- sensory arm begins with specialized sensory receptors called nociceptors
- respond to potential harmful stimuli
- 3 types of stimuli activate nociceptors:
- mechanical:
- thermal:
- chemical:
- inflammatory chemicals make nociceptors more sensitive -\> signal that a damaging stimulus is occurring
- the role of sensory receptors is to convert stimulus energy to electrical energy, which can be conducted down the axons (nerve fibers) of neurons –we call these conducting impulses action potentials
- the nervous system has 2 arms
- Sensory pathways generally consist of 3 neurons in a chain:
- first order sensory neuron –carries action potentials from the sensory receptor to the central nervous system (to either the spinal cord or brain)
- impulse arrives in the dorsal horn f the spinal cord, which is where communication between the first-order & second-order sensory neuron occurs
- second order sensory neuron
- cell body of second-order sensory neurons are located inside the dorsal horn of the spinal cord
- receives information from first-order sensory neuron –the communication occurs at a specialized junction, called a synapse
- signal can be inhibited (not passed on) or passed onto the second order neuron at this point
- nerve fibers of the second-order sensory neurons cross over from one side of the spinal cord to the other
- this cross-over is called d ecussation
- as a result of decussation, signals that originate on one side of the body get carried to the alternate side of the brain
- fibers of second order sensory neurons carry impulses up spinal cord, through the brainstem to the thalamus :
- third order sensory neuron
- cell body of third-order sensory neurons are located in the thalamus (in the brain)
- second-order neuron passes its signal across a synapse to third-order sensory neuron in the thalamus
- fibers of third-order sensory neurons pass upward through the cerebrum to the primary somatosensory cortex
- first order sensory neuron –carries action potentials from the sensory receptor to the central nervous system (to either the spinal cord or brain)
Video 6.2: The Anatomy&Physiology of Pain, Part 2
Two pathways related to our perceptions of pain
- ne pathway involves nociceptor passing signal via a type A delta nerve fiber
- characteristics of these fibers
- large diameter nerve fibers
- fibers are myelinated
- fastest speed of signal transduction
- carry stimulus information related to thermal and mechanical stimuli
- the signals carried by these fibers are perceived as rapid, sharp sensations of pain
- impulse is conducted up through the spinal cord & brainstem in the spinothalamic tract:
- characteristics of these fibers
- The other pathway involves nociceptor passing signal via type C nerve fibers
- characteristics of these fibers
- smallest diameter nerve fibers
- fibers are unmyelinated
- slow speed of signal transduction
- carry stimulus information related to all 3 types of stimuli (thermal, mechanical, chemical)
- the signals carried by these fibers are perceived as dull, burning, throbbing pain
- impulses are conducted up the spinal cord to the brainstem via the spinoreticular tract
- passes up spinal cord to the brainstem, and then on to multiple sites in brain
- adds emotional overtones to perceptions of pain
- characteristics of these fibers
Video 6.3: The Anatomy&Physiology of Pain, Part 3
Three general mechanisms of pain modulation
- ne type of modulation occurs at the level of communication between the first-order and second-order sensory neurons (in dorsal horn)
- ther fibers, called type A beta fibers , are also conducting information to this synapse
- the type A beta fibers are carried in the same nerves that are carrying type A delta fibers & type C fibers
- type A beta fibers (like the type A delta fibers) are large diameter, myelinated fibers (fastest conduction speed)
- type A beta neurons also synapse with second-order sensory neurons –and the impulse/information carried by the second-order neuron is conducted via the spinothalamic tract –and is subsequently carried to the primary somatosensory cortex by third-order sensory neurons
- type A beta fibers carry information related to touch sensation
- ther fibers, called type A beta fibers , are also conducting information to this synapse
- some modulation can also occur because of descending inhibitory pathways
- these pathways originate in brainstem but receive input from other parts of brain
- when activated, an inhibiting signal is passed to dorsal horn
- the signal inhibits transfer of information at the synapse between the first-order and second-order sensory neurons
- thus, there is an inhibition of pain-related input flowing up the spinothalamic and reticulospinal tracts
- these pathways originate in brainstem but receive input from other parts of brain
- the third mechanism of pain modulation is associated with the endogenous opiod system
- the endogenous opiods: enkephalins, endorphins, dynorphin
- piods are analgesics –i.e., they decrease the perception of pain
- in high concentrations in the braintem –there are receptors for the endorphins in the brainstem & spinal cord
Video 6.4: Types of Pain
Three types of pain:
- somatic pain
- can be localized and can often be replicated
- subcategories:
- superficial somatic pain
- typical experienced in response to mechanical or thermal stimuli
- sharp, rapid onset
- deep somatic pain
- typically experience in muscles and joints
- usually perceived as aching, throbbing, burning pain
- superficial somatic pain
- visceral pain
- this types of pain is associated with internal organs, which have nociceptors in their walls
- deep throbbing pain
- impulses related to this type of pain are carried by type C nerve fibers
- through unconscious neural reflexes, this kind of pain can trigger nausea, vomiting and other symptoms
- this type of pain is difficult to localize –is often experienced as referred pain –i.e., brain interprets the pain as occurring at the body surface
- neuropathic pain
- unlike somatic pain & visceral pain, neuropathic pain occurs when nerves themselves are damaged (rather than when nociceptors are activated)
- there are varied reasons for this type of pain:
- diabetic neuropathy
- phantom limb pain
- carpal tunnel syndrome
- nerves compression or trauma
Video 6.5: Assessing Pain Demonstration
-
pain is a subjective experience, so it can be difficult to assess
-
comprehensive pain assessment in a health care setting involves a number of question areas
- intensity
- assessed via pain scales
- verbal scales :
- picture scales-
- Veteran and Defense Pain Scale
- Wong-Baker FACES Scale
- onset
- duration
- frequency
- location
- quality
- examples -burning, aching, sharp, etc.
- associated symptoms
- examples- nausea, shortness of breath
- precipitating factors
- alleviating factors
- impact
- examples- ability to walk, sleep normally, etc.
- intensity
Video 6.6: Social, Cultural & Psychological Influences on Pain
- the history of our understanding of pain-
- until the 19th century: pain was dichotomized as either a somatogenic experience or a psychogenic experience-
- pain was thought of as a linear sensory experience
- in the 20th century- Melzack and Wall developed the gate control theory of pain -
- pain was is both a sensory and emotional experience
- until the 19th century: pain was dichotomized as either a somatogenic experience or a psychogenic experience-
- influence of social factors on pain-
- examples of social factors-
- eduation
- type of work
- income-
- less access to healthcare, less continuity of care, more manual labor
- Rash Portnoi's study-
- examples of social factors-
- pain and culture-
- culture:
- very misunderstood area in terms of pain influence – vast heterogeneity within cultures
- social factors often shape cultural belief structures
- effect of treatment on subsequent pain experiences-
- acute pain is adaptive (i.e., it serves a purpose)
- untreated acute pain may become pathological - chronic pain
- chronic pain is not considered to be adaptive
- puts a strain on psychological reserves and social resources
- certain groups are less likely to receive treatment
Video 6.7: The Treatment of Pain
- treating pain is important for several reasons-
- physicians and nurses make an ethical and professional commitment to decrease suffering and promote comfort
- provides comfort
- short term and long term consequences of untreated pain-
- physiologic consequences-
- functional consequences-
- psychosocial consequences-
- nociceptive signal –is ultimately integrated in multiple areas of the brain
- manifestations are apparent with physiologic monitoring and behavioral changes
- examples- increased blood pressure, decreased movement, grimacing
- best way to assess the pain experience is through the patient's self-report
- sometimes a disconnect with actual pain experience and what is reported –always explore further
- may use a different term for pain-
- may worry about consequences-
- barriers to reporting pain-
- sometimes a disconnect with actual pain experience and what is reported –always explore further
- manifestations are apparent with physiologic monitoring and behavioral changes
- Treating pain-
- goal of therapy is individualized- i.e., patient-focused:
- evaluate risks and benefits of different therapies-
